Introduction: What Is A Subluxation?
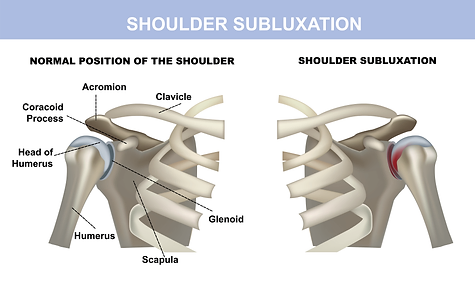
Following the onset of a stroke, it is common that the hemiparetic arm may experience something called a subluxation or “slipped shoulder”. This is a very common impairment that follows in the wake of arm weakness caused by a stroke. Shoulder subluxations occur in the glenohumeral joint of the shoulder. This is the area in which the humerus (bone of the upper arm) inserts into the shoulder near the clavicle. The uniqueness of the humerus includes a lack of ligaments, relying on weakened tendons to support the head of the humerus in the shoulder girdle. Due to a lack of ligaments, the tendons which support the head of the humerus into the joint itself become laxed and lengthened, allowing gravity to pull the head of the joint out of the socket. This in turn causes a subluxation.
Shoulder subluxation can be very frustrating during stroke recovery causing pain due to impingement of nerves, deficits in arm range of motion, atrophy, alignment/posture, mobility, and self-care.
When a shoulder subluxation occurs, the joint can either be anteriorly or posteriorly rotated within the capsule. Rarely, does the joint pull straight down to the ground without some sort of rotation. Anterior rotation refers to the movement of the head of the humerus into a forward position. Adversely, posterior rotation refers to the backward rotation of the joint. When a subluxation occurs, sheering off the head of the humerus within the capsule cause pain due to impingement of the median nerve on which it is rubbing, therefore causing burning pain throughout the entire upper extremity.
How Do You Know If You Have A Subluxation?
Shoulder subluxations following a stroke can occur quickly after a stroke, but most commonly occur chronically due to continued weakness of the arm. Over time, gravity continues to pull the joint apart. A shoulder assessment usually occurs during any post-stroke evaluation which will consider the position of the humerus of the head into the joint. A therapist or physician will be able to check the integrity of the joint. If a subluxation is present, scoring of the separation is based on the distance between the bone and the gap of the top of the shoulder. Sometimes the term “one or two finger separation” is used to describe the severity of the gap. After the assessment of the gap, a physical palpitation (feeling of the joint) is then completed to find if the head of the joint is rotated anteriorly or posteriorly.
How To Avoid And Rehabilitate Subluxations After A Stroke
The most effective way to avoid or prevent a subluxation following a stroke is by functional use and active range of motion of the arm to allow for continued strengthening of the deltoids and surrounding muscles which all help contain the joint into the capsule which is subluxated. Working with an occupational or physical therapist after a stroke is essential for the guidance of appropriate exercises based on the current strength and impairment level of the upper extremity.
Please find below exercises for suggestions of appropriate rehabilitation interventions for the management of shoulder subluxation.
Taping:
Leukotape® and Kinesiotape® can be used to help hold and approximate the head of the humerus into the joint capsule. Taping may be effective to bring the joint out of the anterior or posterior position to increase comfort and stability.
Use Of A Sling for Support:
Shoulder slings provide support under the elbow or at the wrist to assist with an approximation of the joint into the capsule. In general, slings do not offer enough support to keep the joint in the capsule and do not permanently correct anterior or posterior rotation. Slings also may promote tightness of muscles and joint capsules as a result of the arm being rotated inward close to the body. However, slings may provide temporary pain reduction and comfort. It is important to wear slings for shoulder subluxation only when walking or completing transfers for support with mobility or against gravity. Wearing slings constantly is not recommended as it can in turn cause increased tightness of the whole arm due to lack of movement or activity.
Support In the Environment:
Use of an arm prop such as an arm trough on a wheelchair or a pillow placed under the elbow for support while sitting and lying can help provide support to the subluxated joint and increase comfort.
Weight-Bearing Activity:
Weight-bearing is a technique that involves loading muscles and joints for a therapeutic benefit. In the case of subluxation of the shoulder, carefully applied weight-bearing may promote joint approximation and compression of the head of the humerus into the shoulder capsule. This provides proprioception and input to the joint itself to build awareness in positioning.
Passive or Active Range Of Motion Up To 90 Degrees Of Shoulder Flexion: It is important to continue the attempted active or passive range of motion of the affected arm. It is important to bring the shoulder in flexion (front of the body) or abduction (out to the side) only up to shoulder height (i.e. 90 degrees). A passive and active range of motion is essential for the continued prevention of deformities based on tightness and reduced or lack of use of the arm. Bringing a very weak (i.e. flaccid), unstable, or restricted arm past shoulder height can increase the likelihood of nerve impingement and pain and is not recommended.
Practice Good Posture
Slumped over or asymmetrical (leaning over to one side) creates an imbalance in the spine and supportive muscles and joints. This often creates a problem with the shoulder. Try your best to sit tall and not favor one side over the other. Keep this positioning when you use your weaker arm. You may need to seek guidance from physical or occupational therapists to provide exercises to lengthen, strengthen, and improve endurance in certain muscles surrounding the pelvis, lumbar spine, and thoracic spine.
Scapular Exercises:
To improve stability, strength, and mechanics that need to occur for the optimal rhythm of the shoulder and scapula during movement, it is critical to engage in specific scapular exercises. These include, but are not limited to, scapular elevation (e.g. shrugs shoulders), retraction (e.g. squeezing shoulder blades together), and protraction (e.g. moving shoulder blades forward). The movement of the scapula helps to support the surrounding areas of the shoulder and arm to assist with stabilizing the subluxation. Consult a physical or occupational therapist to find out what exercises are going to be most ideal for your clinical presentation
Visual Feedback:
Using a mirror can provide visual feedback for awareness and positioning of the joint. The more awareness the stroke survivor has, the better they will be able to support, position, and correct thought-out all daily activities.
Subluxations can impact the ability of a stroke survivor to focus on the recovery of the upper extremity. This can be due to pain, instability, and interference with the weakened arm’s daily activities. Focusing on protection, stability, and management of joint integrity and pain is necessary to build on activity and functional movement of the affected limb. It should also be noted that there are times when subluxations are not painful. In that instance, it is very important to follow guidelines to manage your shoulder. While pain may not provide a warning to you that damage is being done, you may still be causing injury that will overall limit recovery of the arm and hand.
It is important to talk to your occupational or physical therapist about the daily management of the subluxation. The therapist will need to provide an appropriate examination to make clinical decisions for optimal care and restoration of arm function. Speak to your care team about concerns of a subluxation if you feel that separation has occurred after your stroke.