Hemispatial neglect, also known as left neglect, can occur following a stroke or traumatic brain injury (TBI). Typically, the right side of the brain controls the left side of the body and the left side of the brain controls the right side. Therefore, an injury to one side, or hemisphere, can cause paralysis or weakness on the opposite side of the body (1). This means that an injury to the right hemisphere of the brain can result in left neglect or hemispatial neglect (2).
Those experiencing left neglect may not be aware of everything on their left side. This condition is not the same as a vision loss, but rather a lack of awareness of one side of space due to the brain injury (3). This condition can sometimes be overlooked by healthcare providers, making it important for patients and caregivers to be aware of its signs. The following article will describe the signs and symptoms of left neglect, and strategies that both survivors and caregivers can employ to work through their left neglect.
How Left Neglect Affects a Stroke or Traumatic Brain Injury (TBI) Survivor
Left neglect can occur after brain damage and makes it hard for people to notice or respond to things on their left side, leading to slower recovery and increased risk of accidents.
As a result of a stroke or TBI, the brain can sustain damage. Damage to various regions of the brain can lead to different conditions. Left neglect often occurs as a result of damage to the posterior cortex in the right hemisphere of the brain (4). This condition is characterized by a reduced or complete lack of awareness of the left side of a person as well as their surroundings on the left side.
During rehabilitation, people with left neglect typically recover more slowly than those without this condition. Moreover, people with left neglect are more prone to “slip and fall” accidents which can result in serious injuries (5).
While not commonly listed in literature, there are several subcategories of left neglect that can be assessed to determine if a person has this condition (6):
- Perceptual neglect: This is an inability to perceive anything on the left side,
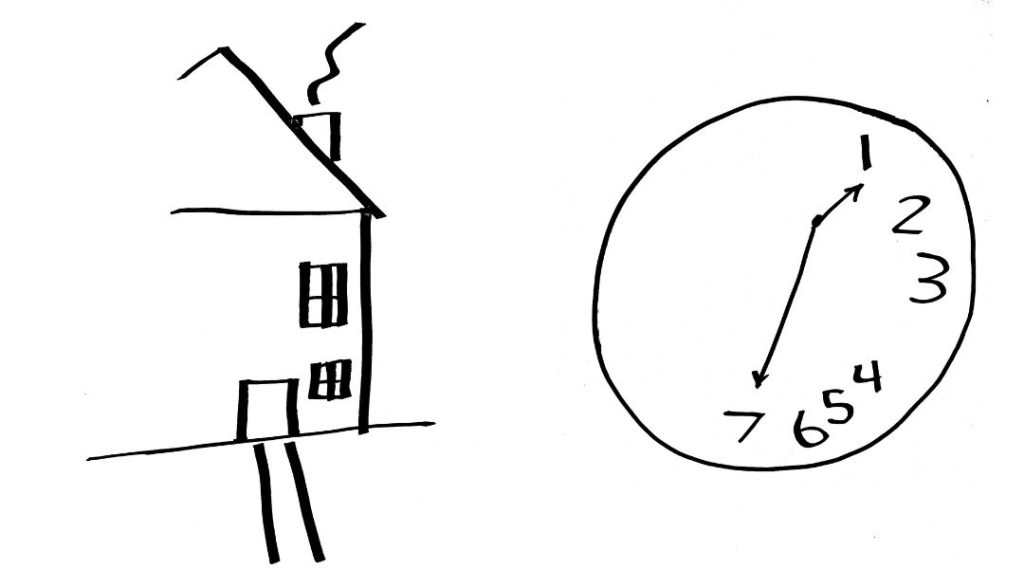
- Representational neglect: This is the inability to imagine or mentally visualize anything on the left side. For example, a person may not be able to picture the numbers on the left side of a clock face.
- Motor neglect: This involves a lack of movement of the left side of the body despite there being no physical reason preventing the movement.
Recognizing the Symptoms of Left Neglect
People with left neglect might experience their brain not recognizing the stimuli on their left side, eat only from the right side of their plate, or bump into things on their left, making them more dependent on others for daily help.
One of the most common symptoms of left neglect in stroke or TBI survivors is when a person turns their head constantly to the right, avoiding the left side altogether. Even though they may feel sensations like heat or pain on the left side of their body, they may not recognize that the left side of the body exists. Other symptoms of left neglect include (7):
- Eating food from only one side of the plate
- Grooming or attempting to dress only one side of the body. An example:

- Drawing a picture of only one side of an object, such as a house that only has the illustration shown on the right. Examples include:
- Accidentally bumping into objects at the left side
- Denying the presence of a person or object on the left side, even after seeing them in the room
Left neglect can be very frustrating for loved ones and caregivers. People with this condition may have frequent outbursts of anger because they are unaware of the problems caused by left neglect and may believe that nothing to their left side actually exists. As a result, those living with left neglect often experience chronic depression and anxiety. Due to the challenges in performing everyday activities, individuals with left neglect are usually highly dependent on others for daily assistance (8).
Left Neglect versus Vision Impairment or “Field Cut” in Eyesight
Left neglect is about a lack of awareness and acknowledgment of the left side, while a field cut is a vision loss from eye or brain damage. Both require different tests and treatments.
Stroke and TBI survivors often experience vision problems immediately following their brain injury unrelated to left neglect. Three of the most common issues are (9):
- Double-vision (seeing double)
- Eye movement problems
- A visual field cut (a blind spot)
The cerebrum, which is the largest part of the human brain, houses the optic nerve. The optic nerve allows us to see and connects the back of the eye to the occipital cortex. If the occipital cortex is damaged, blindness can occur even if the eyes are physically healthy. Additionally, if the injury affects the optic nerve, vision problems can still occur. Around one-third of all stroke victims experience some degree of vision loss (10).
Understanding the Normal Visual Field
A visual field is the entire area a person can see when their eyes are fixed in one position (11). It includes central vision, which is what a person sees directly in front of them, and peripheral vision, which is everything that can be seen to the sides, even from the corners of the eyes. A field cut is an area within this visual field where vision is missing and it is common in people who have had strokes or TBIs. Field cuts are also common in people with other types of neurological conditions.
Type of Field Cuts
Those with optic nerve damage typically experience one of the following types of field cuts (12):
- Homonymous Hemianopia: Loss of vision in either the right or left half of the visual field in both eyes.
- The word “homonymous” comes from Greek, meaning “the same,” so it refers to the same half of vision being lost in both eyes.
- Quadrantanopia: Loss of one-fourth of the visual field in either eye.
- The word “quadrant” comes from Latin, meaning “fourth part,” so it refers to losing a quarter of your vision in one eye.
- Scotoma: A blind spot within the visual field of either eye.
- The word “scotoma” comes from Greek, meaning “darkness,” so it refers to a dark or blind spot in vision.
Additionally, up to 70% of stroke survivors with visual field impairments experience challenges with their central vision (13). Loss of central vision can increase the risk of collisions and injuries because it can make it nearly impossible for a person to see objects directly ahead. This often leads to a lower quality of life for people with visual field cuts, especially those with central vision loss (14).
Key Differences between Field Cuts and Left Neglect
Left neglect is caused by injury to the right posterior cortex of the brain, not by damage to the occipital cortex or with eyesight itself. To determine if a person has vision problems or left neglect, an eye doctor will perform a specific type of eye exam using a pen-light to assess whether there is any optic nerve damage (15). In left neglect, this exam usually shows no optic nerve damage.
Field cuts, on the other hand, are caused by damage to the brain’s occipital cortex or the optic nerve. The location of the field cut determines the specific vision problems a person can experience.
Field cuts can make it difficult to perform daily activities, such as reading and driving. For instance, a person with a field cut might have a car accident because they did not see a stop sign or a pedestrian in the crosswalk. Some survivors with field cuts will frequently move their heads up and down or side-to-side to see objects that are no longer in their field of vision.
A thorough eye exam is crucial for diagnosing field cuts and should be conducted as soon as possible after a stroke or TBI. The sooner a person is evaluated, the sooner a rehabilitation team can assemble a safety plan to help the person manage daily activities. Extra safety measures are especially important, in addition to occupational therapy and/or physical therapy (OT and/or PT), to prevent injuries in those who have decreased eyesight due to field cuts.
Left Neglect Treatment – Therapies and Recovery Strategies
Treating left neglect involves therapies to help people focus on their left side, like special glasses and exercises, which can help them improve and regain independence.
Left neglect can be challenging to treat, but with ongoing effort and therapy, many individuals can make significant progress. A major difficulty in treating left neglect is that many individuals do not realize they have a problem. However, starting treatment as early as possible increases the likelihood of recovery.
One of the main treatment approaches for stroke or TBI survivors with left neglect is the use of specialized glasses during rehabilitation sessions and at home. These glasses are designed to shift the wearer’s visual field, encouraging them to look toward their neglected side (16).
Other primary treatment approaches include (17):
-
- Visual scanning training: This therapy helps individuals consciously pay attention to their neglected side. For example, a therapist may ask the person to locate a large object placed on their left side.
- Active limb activation: This involves exercises that draw attention to the neglected limbs. It can include passive exercises, where a therapist moves the person’s left arm or leg, or active exercises where the person tries to move their limbs independently. For instance, the therapist might lift the person’s left arm above their head in front of a mirror, and then ask them to repeat the movement.
- Sustained attention training: This rehab approach uses devices like an alarm clock or other signaling gadget to help individuals focus attention on their neglected side for a specific period of time. For example, the therapist may ask a patient to gaze at a landscape painting to their left for a specific amount of time and then describe the painting.
Why Left Neglect Treatment is Critical for Overall Recovery
Treatment for left neglect typically occurs within a multidisciplinary rehabilitation approach involving various healthcare professionals such as social workers, OT and/or PT, cognitive therapists, and counselors. When left neglect is not addressed, individuals are more likely to progressively ignore the left side of their bodies and surroundings over time.
Without intensive treatment, left neglect most often becomes permanent and irreversible, leading to the need for daily assistance with self-care activities. Furthermore, it can significantly hinder progress in OT and/or PT, which is aimed at re-learning lost motor skills. Therefore, identifying and treating left neglect is vital for recovery, restoration of independence in everyday activities, and overall well-being.
Strategies to Manage Left Neglect in Daily Life
Family and caregivers can help people with left neglect by positioning themselves on the left, guiding left-hand use, and encouraging awareness of the left side to promote improvement.
Family members, friends, and caregivers of those with left neglect can play an important role in helping them live as independently as possible at home.
Below are three strategies that caregivers can employ:
Positioning Techniques for Improved Left-Side Awareness
Place a chair on the left side of the survivor’s chair or bed and sit in it when interacting with them. This encourages them to look toward their neglected side.
Assistance with Eating: Encouraging Left-Side Use
Guide the survivor’s left hand to hold an eating utensil, and assist them in eating with that hand. This can help increase awareness of use of the neglected side.
Increasing Awareness: Tips for Caregivers
Take every opportunity to draw attention to objects, people, or views on their left side. By consistently increasing awareness of their left side, there is a greater chance of incremental improvement of left neglect symptoms over time.
Key Takeaways on Left Neglect: Insights for Better Understanding and Management
Hemispatial neglect, often called left neglect, results from an injury to the brain’s right posterior cortex. This condition causes a lack of awareness of the left side of the body and surroundings, increasing the risk of accidents. In stroke and TBI survivors, the presence of left neglect can delay diagnosis and treatment, hindering progress in OT and/or PT and overall recovery. Cognitive impairments, such as difficulties with attention and memory can further complicate treatment (19).
Early treatment in a multidisciplinary rehabilitation setting significantly improves the chances of recovery from left neglect. By addressing left neglect promptly and comprehensively, stroke and TBI survivors are more likely to regain personal independence in daily activities and experience a better quality of life.
References:
- Johns Hopkins Medicine [Baltimore, MD]. Effects of Stroke. Webpage: https://www.hopkinsmedicine.org/health/conditions-and-diseases/stroke/effects-of-stroke
- Sarwar A, and Emmady PD. (2023). Spatial Neglect.. In: StatPearls [Internet]. StatPearls Publishing: Treasure Island, FL. Webpage: https://pubmed.ncbi.nlm.nih.gov/32965855/
- American Stroke Association. Visual Disturbances. Webpage: https://www.stroke.org/en/about-stroke/effects-of-stroke/physical-effects-of-stroke/physical-impact/visual-disturbances#:~:text=About%2030%25%20of%20stroke%20survivors,several%20areas%20in%20both%20eyes.
- Sarwar A, and Emmady PD. (2023). Spatial Neglect.. In: StatPearls [Internet]. StatPearls Publishing: Treasure Island, FL. Webpage: https://pubmed.ncbi.nlm.nih.gov/32965855/
- Campbell GB, and Matthews JT. (2010). An integrative review of factors associated with falls during post-stroke rehabilitation. Journal of Nursing Scholarship 42(4): 395-404. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4465217/#:~:text=demonstrated%20that%20hemineglect%20increased%20the,did%20nonfallers%20(64%25%20vs.
- Williams LJ, Kernot J, Hillier SL, et al. (2021). Spatial Neglect Subtypes, Definitions and Assessment Tools: A Scoping Review. Frontiers in Neurology 12:742365. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8653914/
- Li K, and Malhotra PA. (2015). Spatial neglect. Practical Neurology 15(5): 333-339. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4602245/
- Wang W, Zhang X, Ji X, et al. (2015). Mirror neuron therapy for hemispatial neglect patients. Scientific Reports5: 8664 Webpage: https://www.nature.com/articles/srep08664
- Rowe FJ, Hepworth LR, Howard C, et al. (2019). High incidence and prevalence of visual problems after acute stroke: An epidemiology study with implications for service delivery. PLoS One 14(3): e0213035. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6402759/
- Stroke Foundation. Vision loss after stroke. Webpage: https://strokefoundation.org.au/what-we-do/for-survivors-and-carers/after-stroke-factsheets/vision-loss-after-stroke-fact-sheet#:~:text=About%20one%2Dthird%20of%20stroke,few%20months%20after%20a%20stroke.
- Spector RH. (1990). Chapter 16 – Visual Fields. In: Walker HK, et al (Editors). Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd Edition. Butterworths: Boston, MA. Webpage: https://www.ncbi.nlm.nih.gov/books/NBK220/
- American Stroke Association. Let’s Talk About Stroke and Vision Changes. Webpage: https://www.stroke.org/en/help-and-support/resource-library/lets-talk-about-stroke/vision-changes
- Rowe FJ, Hepworth LR, Howard C, et al. (2019). High incidence and prevalence of visual problems after acute stroke: An epidemiology study with implications for service delivery. PLoS One 14(3): e0213035. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6402759/
- Cloutier M, and DeLucia PR. (2022). Topical Review: Impact of Central Vision Loss on Navigation and Obstacle Avoidance while Walking. Optometry and Vision Science 99(12): 890-899. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9813875/#:~:text=Restricted%20mobility%20due%20to%20central,as%20depression%2C13%20and%20anxiety.&text=Central%20vision%20loss%20also%20is,by%20collisions%20with%20other%20objects.
- Bruegger D, Grabe HM, Vicini R, et al. (2023). Detection of Relative Afferent Pupillary Defects Using Eye Tracking and a VR Headset. Translational Vision Science and Technology 12(6): 22. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10309159/
- Goedert KM, Zhang JY, and Barrett AM. (2015). Prism adaptation and spatial neglect: The need for dose-finding studies. Frontiers in Human Neuroscience 9: 243. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4415396/
- Barrett AM, and Houston KE. (2019). Update on the Clinical Approach to Spatial Neglect. Current Neurology and Neuroscience Reports 19(5): 25. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6733261/
- American Stroke Association. One-Sided Neglect. Webpage: https://www.stroke.org/en/about-stroke/effects-of-stroke/vision-and-hearing/one-sided-neglect
- Mulhern M. (2023). Cognitive Rehabilitation Interventions for Post-Stroke Populations. Delaware Journal of Public Health 9(3): 70-74. Webpage: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10494803/