The Function of the Motor Cortex
In recent years, the field of neurorehabilitation has undergone a paradigm shift and a fundamental change in the approach to therapy supporting motor cortex damage following a stroke or neurological dysfunction. It is now clear that the damaged brain compensates in a variety of ways following an injury.
Motor Cortex and Strokes
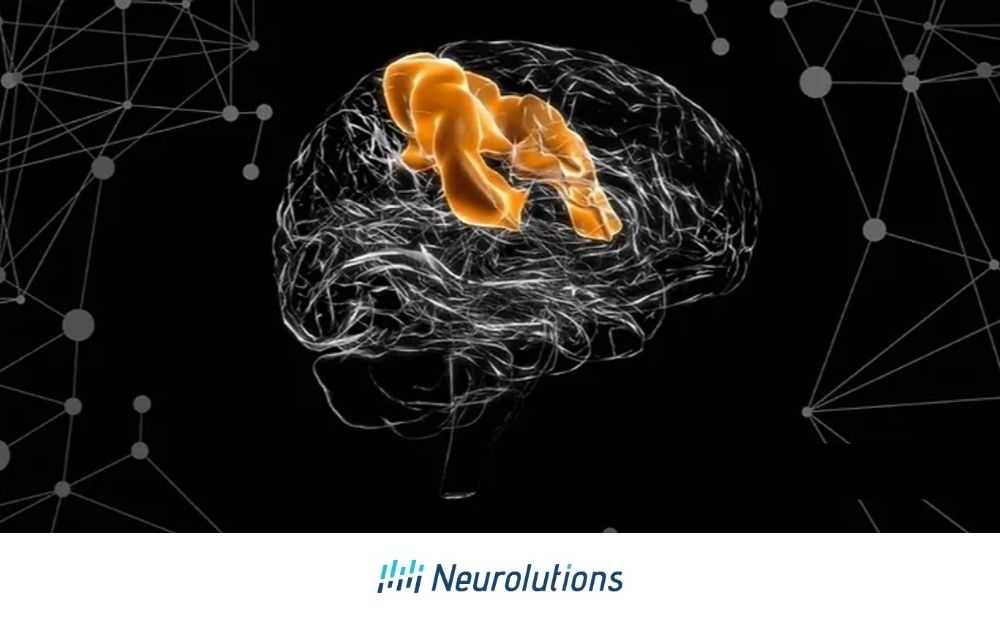
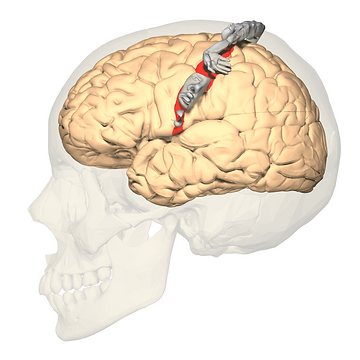
The motor cortex is composed of several interconnected intracortical regions that are from their surrounding areas. There is the primary motor cortex, also known as “M1” located in the precentral gyrus as well as the premotor cortex (PMd) and the supplementary motor (SMA) area, and the cingulate motor cortex (CM) located on the anterior (front) paracentral lobule on the medial (middle) surface of the brain.
Figure 1: Polygon data were generated by Database Center for Life Science(DBCLS)[2]., CC BY-SA 2.1 JP <https://creativecommons.org/licenses/by-sa/2.1/jp/deed.en>, via Wikimedia Commons
The primary motor cortex (M1) is responsible for the direction of movement of the body. Several neurons in the primary motor cortex are selective for particular directions of movement. For example, one cell may fire to move the hand to the right and then it may inhibit (or stop the firing of signals) when moving the hand in the opposite direction. In totality, the motor cortex is responsible for the planning, control, and execution of voluntary movements such as walking or reaching for a cup to bring to our mouth and then take a drink.
Effects of Stroke on Motor Cortex
Plasticity in the motor cortex organization as a result of motor skill learning has also been shown in rehabilitation following a stroke occurs during skills-dependent changes during the acquisition of motor tasks.
When a stroke occurs, this can impact the ability of the motor cortex to direct functional movement. Disruption to the motor cortex may not only cause weakness but also decreased the ability to plan how to move the body part itself. The timing of learning motor tasks may be crucial during recovery as some studies show that for example, learning to take steps in sequential order may send more blood flow to the motor cortex.
Studies also suggest that new motor learning occurs with at least 7-10 days of rehabilitation but not within 3 days, once again demonstrating the need to implement mass repetition of movements following stroke and the importance of continuing to use the affected extremities as much as possible following a stroke.
How to Retrain the Brain
Following a stroke, it is important to look at the effect of skill learning with repetitive and nonskilled motor activity. There are three general principles or theories that have been proposed to explain recovery following stroke or damage to the motor cortex. They are as follows: 1) reversal of diaschisis, 2) compensation, 3) adaptive plasticity.
Reversal diaschisis is the temporary reduction in the function of areas associated with the injured area of the brain in the acute stage of recovery. Blood flow and metabolism are reduced to the area of injury in the brain following a stroke and gradually return to the connected regions.
Because this disruption is temporary, healing of the brain can help regain function in the affected limbs. Therefore, a stroke survivor who was unable to move their arm at the time of the stroke may demonstrate increased arm movement after medical treatment in the hospital without the introduction of therapy or functional use of the arm. This may also be referred to as spontaneous recovery. Spontaneous recovery is usually incomplete and highly variable from person to person. It serves to return function to the injured but surviving neural matter.
Compensation refers to the attempt to supplement lost functions with alternative strategies such as using a different part of the body to complete a task (using the non-affected limb to brush teeth) or adaptive equipment such as an electric toothbrush instead of a traditional one to make the rotation of the object easier. When using compensation, fewer changes occur in the motor cortex when not using the impaired limb or limbs. It is not favorable to lean on compensatory techniques in the acute stages of recovery
Adaptive plasticity otherwise known as neuroplasticity occurs when underlying mechanisms and existing connections in the damaged part of the motor cortex or surrounding areas form new connections in regions of the brain through a functional activity which can then lead to greater functional improvement. Actions that support active plasticity are the mass repetitive practice of skills, performing tasks that are meaningful and engaging to the individual, and training intensively.
Overall, treatment of upper extremity impairments following includes neurofacilitation and functional retraining. The use of these techniques can be partially based on the stage of recovery in which the stroke survivor is in. Traditionally therapy has focused on the prevention of compensatory strategies in the acute phase of stroke in order to minimize maladaptive strategies and facilitate neuroplasticity recovery, whereas the choice stages have usually focused on the teaching of compensatory strategies due to long-standing deficits and less likely recovery. However, with the use of new technologies, such as brain-computer interface, the paradigm shift of this thinking can allow the use of neuroplasticity rehabilitation techniques in the chronic stages of stroke recovery and rehabilitation to improve functional outcomes for upper extremity use.
References:
Brain injury medicine: principles and practice. Zasler et al. Demos Medical Publishing, an imprint of Springer Publishing. New York, 2013