Following a stroke, some survivors may notice a change in mood or ability to manage emotions. This is a common side effect of stroke and is also amplified depending on the location in the brain in which the stroke occurred. It is estimated that 32-61% of individuals who have experienced a stroke experience depression or some other type of change in emotions.
Mood changes can be due to damage to the area of the brain which regulates behavior, or it can be due to a difference in physical or cognitive ability leading to feelings of depression or being withdrawn. Changes in mood can also be affected by impairments following strokes such as decreased memory, initiation, language processing, and visual perception. In turn, this can cause confusion, leading to anger and outbursts.
Common Changes Seen In Emotions After Stroke Include The Following:
Depression
- Persistent feelings of sadness or loss of interest in an activity. Unable to pull one’s self out of feeling sad. Some survivors may communicate this as feeling hopeless or wanting to give up following a stroke.
Anxiety
- Characterized by worry, nervousness, or unease, typically about an upcoming activity or something with uncertain outcomes. Some stroke survivors may also present with preservations (i.e. inability to stop thought or activity) surrounding anxious feelings.
Impulsiveness
- Can be motor or cognitive in nature and characterized by the inability to inhibit or limit risky behavior.
Paranoia
- Characterized by suspicion and mistrust of people or their actions without evidence or justification. Can be delusional in nature. Seen acutely or during hospitalization following a stroke
Pseudobulbar Affect
- Occurs when there is a misconnection between the frontal lobe (i.e. area of the brain which controls emotions) and the brain stem. It is characterized by sudden bouts of anger, crying, or laughing not matching the situation. Some of the outbursts can last a few seconds to a long time.
Flat Affect
- Showing almost none to no emotion at all in situations in which individuals usually experience emotions such as joy, sadness, etc.
Inappropriate Affect
- Exhibiting behavior or emotion that does not match the situation
Grief
- Deep sorrow is experienced after a loss. After a stroke, this grief may be connected due to loss of independence or change in roles or abilities.
Personality Changes
- Apathy, irritability, or social withdrawal can also be seen after a stroke
When these behaviors or emotions are typical for the individual who has experienced a stroke, the emotions can be exacerbated (increased or highlighted). This is especially true for individuals such as veterans with a history of post-traumatic stress disorder (PTSD) or other groups of people such as substance abuse, bipolar disorder, or schizophrenia. A history of disenfranchisement can lead to a lack of trust in the medical team, limiting services to refusal, anxiety, and paranoia surrounding services and treatment. It can be imperative to implement strategies for coping mechanisms in order to help the survivor if he or she is someone who already has a history of any of the above symptoms or a history of mental illness.
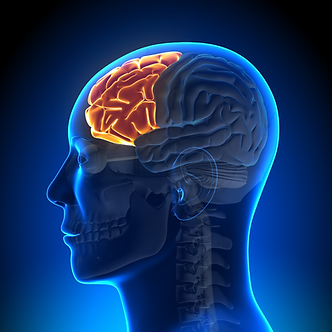
Areas most commonly affected and which can cause changes in the brain following a stroke are as listed below:
- Frontal lobe: lability, perseveration, impulsiveness, memory deficits, judgment, social awareness, and overall main area of the brain responsible for the regulation of emotions
- Parietal lobe: frustration
- Midbrain, thalamus, and caudate nucleus- agitation, hallucination, memory loss, alteration in arousal, confusion
It is essential to educate the stroke survivor caregivers and individuals who work with them or interact with them on a regular basis on changes that have occurred and the best way to interact with the behavior before becoming interfering.
A supportive approach can be helpful by acknowledging that the individual has suffered a sudden and dramatic life change with a shift in role and ability to take care of themself. A limitation of some recovery is denial or perseveration on regaining full recovery rather than focusing on small steps toward improvement
Some interventions are the following to help with each factor of behavior:
Decreased Memory After Stroke Affecting Mood And Behavior
- Using written reminders to help with memory
- Writing out steps to correctly sequence an activity
- Limiting distractions in order to lessen confusion and frustration during a task
- Promoting engagement in activities in which the survivor can be successful in order to build self-esteem and routine in the activity to increase independence
- Use of timers as reminders to build independence
- Skilled intervention with occupational therapy and speech therapy
- If language is impaired, keeping instructions short and simple helps to decrease frustration
Impulsiveness/Lack of Judgment after Stroke
- Keeping the same/similar daily schedule to increase independence with daily activities
- Use of timers to limit activity participation
- Skilled intervention with occupational therapy and speech therapy
- Redirecting of behavior
- Keeping activity short and simple to limit overstimulation in-turning creating impulsivity
- Practicing safe scenarios in the home and community
- Preparation of safe activities in which the individual can participate
Depression after Stroke
- Medication
- Cognitive behavioral therapy with a trained professional
- Encourage participation in social support networks such as family, friend, or support groups if this fits their needs
- Allow success in daily activity to encourage independence in activity
- Continuing to offer choices and treat them as an individual/adults although the person may no longer have the ability to make large decisions for themselves
Pseudobulbar Affect or Other Inappropriate Social Interactions
- Redirect behavior
- Walk away or actively ignoring of behaviors until the behavior has calmed if safe to do so
- If appropriate, provide feedback to the individual that the behavior is not appropriate and then educate them on what is the appropriate response
- Practice communication and conversations
Anxiety or Perseverations On Thoughts Or Activities
- Cognitive behavioral therapy with a trained profession
- Setting limits
- Writing out realistic solutions and goals to problems
- Working with a social worker for increased community support
Paranoia after Stroke
- Medication intervention
- Cognitive behavioral therapy with a trained professional
- Use of clear simple language with expectations
- Use of a set/similar daily routine
- Staying in a familiar or safe environment which is support of individual needs
- Use of signs or reminders of people and environment
Please speak with your physician or medical professional for medical and behavioral intervention. This information is an overview of common changes after a stroke and is not meant to replace medical advice.
References:
- American Stroke Association.
- Websters dictionary
- Bakhshani NM. Impulsivity: a predisposition toward risky behaviors. Int J High Risk Behav Addict. 2014 Jun 1;3(2):e20428. doi: 10.5812/ijhrba.20428. PMID: 25032165; PMCID: PMC4080475.
- Pendleton and Schulta-Krohn (2006) Pedretti’s Occupational Therapy Practice For Physical Dysfunction: 6th Edition. New York, Elisver.