Hemiparesis is a common after-effect of a stroke that causes weakness on one side of your body. This condition affects about 8 out of 10 stroke survivors (1). It is important to know the severity of your stroke and the location of where the stroke occurred to get a better understanding of your hemiparesis. For instance, if you experienced a stroke on the right side of your brain, then you would experience weakness on the left side of your body. Knowing more about your stroke will help you make a successful recovery plan and live an enjoyable life.
One-sided weakness can limit your movement, which can affect your activities of daily living, social participation, work, and even your leisure activities. In this article, you will learn more about symptoms, causes, and how to live with hemiparesis after surviving a stroke.
What is Hemiparesis?
Hemiparesis is defined as partial weakness of one side of the body. This condition may affect the arms, hands, legs, face, neck, and/or your trunk. In some cases, hemiparesis may involve a combination of body parts (1).
Many stroke survivors and care-partners get confused between the term hemiparesis and hemiplegia. Hemiparesis speaks to weakness of one side of the body, while hemiplegia is the paralysis of one side of the body. Both conditions are dependent on where the stroke occurred in the brain.
Causes of Hemiparesis
What might cause hemiparesis? During a stroke, certain parts of your brain do not get enough oxygen due to the disruption of the blood supply, causing brain cells to die. If these cells are associated with body strength, coordination, and movement, then damaging them can cause hemiparesis (4). Each hemisphere of the brain controls movement of the opposite side of the body, which is why hemiparesis will be on the opposite side of the damaged side of the brain when you experience a stroke.
If you have a stroke that occurs in the left side of the brain, the right side of your body will have hemiparesis. You may experience difficulty in talking and understanding (aphasia), in addition to knowing the difference between left and right. If you experienced a stroke that occurred in the right side of the brain, then you will experience hemiparesis on the left side of your body (4). You may experience ataxia (i.e. difficulty in coordinating movement), which will lead to a loss of balance and difficulty in walking. For additional information, visit A Guide to Right vs. Right Strokes.
These conditions can be caused by an ischemic stroke, which is when blood supply is cut off. In the case of a hemorrhagic stroke, the brain experiences bleeding from blood vessels rupturing. Less commonly a stroke survivor may experience a stroke that causes ipsilateral hemiparesis: weakness on the same side as the injury. The location of where the stroke occurred in the brain will determine the location of your weakness. Strokes can also occur outside of the hemispheres of the brain within the cerebral cortex. For more information on these types of strokes, visit our blogs to read more within the following articles: Pontine Strokes, Basal Ganglia Strokes, Cerebellum Strokes.
Symptoms of Hemiparesis
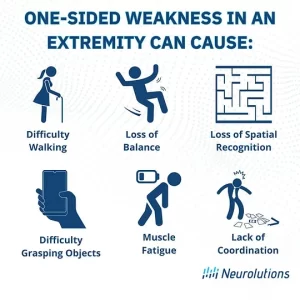
Some symptoms of hemiparesis include (3):
- Loss of balance
- Difficulty walking
- Impaired ability to grab objects
- Decrease in movement precision
- Muscle fatigue
- Lack of coordination
(3)
Mental Practice
There are other treatments that do not include movement therapy, such as mental practice therapy (2). This type of therapy involves mentally rehearsing specific activities to improve performance. This is more of a cognitive treatment instead of a physical treatment for hemiparesis. Mental practice helps activate neuroplasticity and triggers cortical changes. Evidence shows that combining mental practice with physical movement therapies such as physical and occupational therapy produces improved results.
For more information on mirror therapy, mental practice, and other motor priming exercises for hemiparesis, refer to 5 Powerful Brain Exercises for Stroke Rehab.
Medication and Hemiparesis
In some cases, your medical doctor may prescribe you medication to help with muscle spasms, muscle spasticity, and pain. For example, your medical doctor may recommend botox to help with spasticity. Botox is a “nerve block” that blocks the signals causing muscle contraction. It is an injectable treatment that may provide relief for about 3 months. During this period in which your muscles are relaxed, you can focus on rehab exercises to help rewire the brain and address the root cause of hemiparesis (2).
Baclofen is a type of medication that helps relax spastic muscles. While it provides a temporary relief of spastic muscles, it can offer a window of opportunity to pursue intense rehab exercises (2).
Hemiparesis Prognosis
Hemiparesis is different for everyone. Every brain is wired differently, and every stroke impacts different neural pathways. In some cases you can have hemiparesis for a few months, a few years, or you may have it chronically. Not knowing how long you may experience hemiparesis can prove challenging in predicting recovery outcomes and timing. However, after a stroke, the brain enters a phase of heightened neuroplasticity as it attempts to rapidly heal from injury. When this phase slows down, the brain enters a “plateau” phase. This plateau often occurs at the 3-month mark. Many stroke survivors make incredible gains during this time, especially while participating in therapy programs. Beyond the 3-month mark, recovery can become contingent. Stroke survivors tend to remain at the same level of ability. However, when rehab is continued even after stopping for months or years, recovery can continue and you can get stronger (2). Visit Recovery Timelines after Stroke and Chronic Stroke Recovery for encouraging education on how to recover throughout all time ines post stroke recovery.
Coping with Hemiparesis
Experiencing hemiparesis may be challenging and frustrating, however there are tools and strategies to assist in living with hemiparesis. Discussing with your care-partner, loved ones, and medical team will help you the right stroke recovery plan for you.There are different coping techniques to help during stressful times in your recovery. For example, mindfulness and meditation can help reduce the anxiety and stress that is involved in your stroke recovery. Moreover, lifestyle changes can help you recover and increase your quality of life.
Lifestyle changes can include (5):
- Be active and maintain movement
- Strengthen leg muscles and balance through exercises
- Wear flat, wide-toed shoes
- Use prescribed assistive devices (Do not furniture surf)
- Pay close attention while walking
Lastly, home modifications can help reduce anxiety and improve your safety in your home. Home modifications can include (5):
- Grab bars
- Ramps
- Raised toilet seats
- Tub bench
- Hand-held shower head
- Long-handled brushes or washing mitts with pockets for soap
- Electric toothbrushes and razors
- Plastic adhesive strips on the bottom of the bathtub
Make sure you take your time to complete activities. There is no rush in performing your self-care tasks. Ask for help if you get frustrated or if you feel that it is taking too long to perform your tasks. Living with hemiparesis can impact your activities of daily living; however, asking for help and taking your time will improve your quality of life.
Living with hemiparesis can provide a different outlook on life. You are going to perform activities in a different way than how you used to perform them, and that is okay! Discussing your stroke recovery plan with your medical team and care-partner is very crucial. You are in control of your life and the way you want to live it! It may be different now, but that doesn’t mean you cannot live a successful life. There are many techniques and strategies to help you increase your quality of life. Advocate for yourself and speak up on what you want to accomplish in your life. Be sure to visit Blogs at Neurolutions for educational resources on living with hemiparesis.
References:
- https://www.stroke.org/en/about-stroke/effects-of-stroke/physical-effects-of-stroke/physical-impact/hemiparesis (1)
- https://www.flintrehab.com/hemiparesis/ (2)
- https://www.northwell.edu/neurosciences/conditions/hemiparesis (3)
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5946362/ (4)
- https://www.flintrehab.com/activities-of-daily-living-after-stroke/ (5)
- https://www.healthline.com/health/hemiparesis-vs-hemiplegia#diagnosis (6)
- https://youtu.be/1BnsQO7a4Og (7)
- https://strokefoundation.org.au/media-centre/stroke-stories/coping-with-hemiplegia-and-hemiparesis (8)
- https://www.raynersmale.com/blog/2014/12/28/sensation-testing-for-patient-with-central-nervous-system-lesion (9)